|
What is Deep Vein Thrombosis?
Deep vein thrombosis (DVT)
is a condition in which blood clots form in a vein deep within the
body. The word thrombosis means forming a blood clot. The clot itself
is called a thrombus.
A blood clot is a jelly-like mass of congealed
blood. Clotting is the normal way the body stops bleeding and begins
healing following injury. Once the clot has done its job, the body
absorbs it. Sometimes, however, blood clotting can prove harmful.
DVT occurs when a blood clot forms in a deep
vein and remains there.
DVT usually involves the formation of a large clot in the deep veins
in the lower legs and thighs. In rare instances, DVT can occur in
the area around the armpit and collar bone (axillary-subclavian
vein thrombosis), in the upper arm, abdomen, or pelvic region.
It is a dangerous condition because the clot
may become dislodged from the vein and travel inside the vein all
the way to the lung, where it may get trapped and block a vessel
in the lung. This is called pulmonary embolism, which can be deadly.
Deep vein thrombosis most often
occurs in:
|
|
Hospitalized patients
following surgery. |
|
|
Individuals confined
to bed for prolonged periods. |
|
|
Healthy individuals
whose legs remain immobilized for long stretches of time,
such as passengers on lengthy airline flights. |
Causes & Risk Factors
|
|
Immobility |
|
|
Previous Deep
vein thrombosis |
|
|
Major Surgery |
|
|
Pregnancy |
|
|
Oestrogen therapy |
|
|
Oral contraceptives |
|
|
Extended air travel |
|
|
Malignancy |
|
|
Blood disorders |
|
|
Heart disease |
|
|
Injury to leg |
|
|
Paralysis |
Signs & Symptoms
|
|
Calf pain + Swelling
+ Redness |
|
|
Homan’s sign |
|
|
Ankle oedema |
|
|
Varicose veins |
|
|
Venous gangrene |
Differential Diagnosis
|
|
Muscle strain or tear |
|
|
Ruptured Baker’s
cyst |
|
|
Calf muscle abscess |
|
|
Haematoma |
|
|
Lymphangitis |
|
|
Lymphatic obstruction |
|
|
Cellulitis |
Diagnostic Test
|
|
B-mode USG |
|
|
Venous duplex scan |
|
|
Plethysmography |
|
|
D-dimer |
|
|
MRI Venography |
|
|
Venography |
Thrombophilia screen test
|
|
Thrombin-antithrombin
III |
|
|
Fibrinopeptide A |
|
|
Fibrin monomer |
|
|
Protein C |
|
|
Fibrin & fibrinogen
degradation products |
|
|
Tissue plasminogen |
|
|
Platelet factor 4 |
|
|
Beta-thromboglobulin |
|
|
Circulating platelet
aggregates |
|
|
Plasminogen activator
inhibitor activity |
|
|
Protein S |
|
|
Lupus Anticoagulant |
|
|
Factor V Ladien |
Complications
|
|
Pulmonary embolism |
|
|
Post thrombotic leg
syndrome |
Treatment of Deep Vein Thrombosis
|
|
Anticoagulation |
|
|
Thrombolysis |
|
|
Thrombectomy |
|
|
IVC filter |
|
|
Venoplasty |
|
|
Stenting |
Outcome
|
|
Complete spontaneous
lysis of large venous thrombi is uncommon, even in patients
treated with heparin. Only 10 % lyse completely. |
|
|
Complete lysis however
occurs in asymptomatic calf vein thrombi. |
Duration of anticoagulation in DVT
|
|
Transient cause and
no other risk factor: 3 months |
|
|
Idiopathic: 3-6 months |
|
|
Ongoing risk; eg. Malignancy:
6-12 months |
|
|
Recurrent PE/DVT: 6-12
months |
|
|
Pts. With high risk
of recurrent thrombosis exceeding risk of anticoagulation: indefinite |
Ilio-femoral Venous Thrombosis
|
|
Primary focus –
Preventing Pulmonary embolism. |
|
|
Secondary focus –
Preventing post thrombotic leg syndrome |
Intervention
|
|
Thrombectomy |
|
|
Thrombolysis |
|
|
Purpose – Early
and complete removal of thrombus to preserve valve function
and remove obstruction. |
|
|
PTLS occurs due to obstruction
& reflux leading to venous hypertension |
|
|
|
|
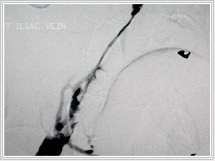
Before Thrombolysis
|
After Thrombolysis
|
|
|
|
|
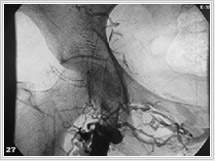
Thrombolysis
|
Thrombolysis
|
|
|
|
|
Thrombolysis
|
Thrombolysis
|
|
|
|
|
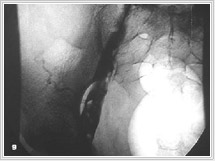
Venoplasty
|
Venoplasty
|
Thrombolytic therapy
Pharmacologic dissolution of thrombus
from the deep venous system appears to be an ideal goal of treatment
which has the potential of eliminating deep venous obstruction and
maintaining valvular function.
Catheter directed thrombolysis
|
|
In acute DVT < 10
days. |
|
|
Urokinase 150,000 U/hr
via multi-sidehole catheter. |
|
|
Heparin 500 U/hr. concomitantly
via popliteal sheath |
|
|
Venograms every 12 hrs
to reposition infusion devices |
Thrombolytic vs Heparin Therapy
Thirteen studies are reported in the literature
which compared anticoagulation therapy to thrombolytic therapy for
acute deep venous thrombosis. Of the patients treated with thrombolytic
therapy, 45% had significant or complete clearing on post-therapy
phlebography compared to only 4% of those treated with heparin.
Venous Thrombectomy
|
|
Many vascular surgeons
are reluctant to apply these techniques in clinical practice.
|
|
|
Pooled data from contemporary reports of iliofemoral
venous thrombectomy indicate that the early and long-term
patency of the iliofemoral venous segment is approximately
80%, contrasted to only 30% of patients treated with anticoagulation
alone.
|
Success
|
|
Thrombectomy - 75% |
|
|
Thrombolysis - 80% |
Indications for IVC filter
|
|
PE with contraindication
to anticoagulation |
|
|
Recurrent PE despite
adequate anticoagulation |
|
|
DVT with free floating
Thrombus |
|
|
Prophylaxis for orthopaedic
trauma |
Pregnancy and DVT
|
|
Normal pregnancy is
a hypercoagulable state. |
|
|
LMWH does not cross
placenta and is not secreted in breast milk. |
|
|
LMWH should be continued
throughout pregnancy and stopped before delivery. |
|
|
Anticoagulation- restarted
in puerperium and continued for 6 weeks to 3 months |
Recurrence
|
|
DVT recurs in 5-10%
of pts. The year after ACT is discontinued and 30 % after 8
years. |
|
|
Post thrombotic leg
syndrome occurs in 50% of pts. with symptomatic DVT. With improved
treatment it has decreased to 30 % after 8 years of follow-up. |
FAQ
Q. Who is at risk for deep vein thrombosis?
A. Some people are more likely than
others to develop thrombosis. Those at risk include:
|
|
The elderly |
|
|
Diabetics |
|
|
People with blood disorders |
|
|
Women who take oral
contraceptives (birth control pills) or other medications
that contain the hormone estrogen |
|
|
People with a history
of thrombosis |
|
|
People who have just
undergone major surgeries or have just suffered a bone fracture.
|
Facts about deep vein thrombosis:
|
|
Deep vein thrombosis
is the second most common vascular problem in the World. The
first is varicose veins. |
|
|
In India, deep vein
thrombosis affects as many as 600,000 individuals every year. |
|
|
The condition
is most commonly seen in people over age 60, but anyone can
be affected. |
Unfractionated Heparin
Unfractionated heparin (UFH) has been
used for over 50 years in the prevention and treatment of thrombosis.
For the treatment of deep-vein thrombosis (DVT) and pulmonary embolism
(PE), it is administered by intravenous infusion (i.e. it is infused
over a period of time into your vein) and has a rapid anticoagulant
effect. You have to be in hospital to receive this treatment. Low-dose
UFH is commonly used for prevention of thrombosis (thromboprophylaxis)
in patients who are undergoing general surgery, but it is less effective
than other forms of prevention in high-risk patients who are undergoing
major orthopedic surgery (e.g. hip or knee replacement surgery).
|
|
Side effects
|
| |
UFH is associated with a risk of bleeding,
heparin-induced thrombocytopenia (low platelet count in
the blood) and local reactions in the skin around the site
of infusion. Long-term use of UFH may also be associated
with an increased risk of osteoporosis (loss of bone tissue
leading to brittle bones). If you experience any side effects,
you must consult your physician.
|
|
|
Potential drug interactions
|
| |
Before you start taking UFH, you may
be asked to stop taking any other treatments that may increase
your risk of bleeding (e.g. other anticoagulant and platelet
inhibitors, such as aspirin or nonsteroidal anti-inflammatory
drugs). If your physician considers it is necessary for
you to continue taking these treatments while you are taking
UFH, he/she is likely to ensure that you are monitored very
carefully.
|
|
|
Monitoring of therapy
|
| |
If you are receiving treatment with UFH,
the dose you receive has to be regularly monitored and adjusted
to ensure that you are sufficiently protected from thrombosis
forming in your veins. Your physician will conduct a blood
test (the activated partial thromboplastin time, or aPTT,
test) 6 hours after the first dose and at least once a day
thereafter to ensure that you are receiving the correct
dose of UFH.
|
Low-molecular-weight heparin
Low-molecular-weight heparin (LMWH)
is derived from unfractionated heparin (UFH). It is injected under
the skin (i.e. subcutaneous injection) and has a rapid anticoagulant
(anticlotting) effect. LMWH has several advantages over UFH, including
a predictable response to the dose of drug and a longer-lasting
effect. This means that it can be administered only once or twice
a day. It is also more convenient to inject under the skin than
into a vein, which means that you may be able to inject yourself
at home rather than having to go to hospital. LMWH is a highly effective
and generally safe form of prevention (thromboprophylaxis) and treatment.
|
|
Side effects
|
| |
LMWH is associated with a small risk
of bleeding (most commonly minor bleeding), thrombocytopenia
(a low platelet count in the blood) and osteoporosis (loss
of bone tissue leading to brittle bones). These side effects
with LMWH are rare, with bleeding being the most common,
but if you experience any side effects, you must consult
your physician.
|
|
|
Potential drug interactions
|
| |
Before you start taking LMWH, you may
be asked to stop taking any other treatments that could
increase your risk of bleeding (e.g. other anticoagulant
and platelet inhibitors). If your physician considers it
is necessary for you to continue undergoing these treatments
while you are taking LMWH, he/she is likely to ensure that
you are monitored very carefully.
|
|
|
Monitoring of therapy
|
| |
LMWH is injected at a fixed dose decided
in accordance with your weight. There is no need for your
physician to monitor or adjust the amount of drug injected
once the correct dose has been found (using a blood-clotting
test), unless you are pregnant, have kidney failure, weigh
more than 100 kg, or are a child.
|
Oral anticoagulants
The oral anticoagulant warfarin
has been used successfully for over 50 years in the prevention of
thrombosis.
Warfarin is not recommended for the prevention
of thrombosis in patients who are undergoing general surgery. Warfarin,
dose-adjusted according to the results of a blood clotting test,
is generally safe and effective in the prevention of thrombosis
in patients who are undergoing major orthopedic operations (e.g.
hip or knee replacement surgery).
Treatment of thrombosis using warfarin is usually
started while you are in hospital and can be continued after you
are discharged. Warfarin is generally safe; however, it is not effective
until at least 3 days after you have taken it and it is only effective
within a narrow range of doses (called a therapeutic window). For
this reason, when you are first diagnosed with a deep-vein thrombosis
(DVT) or pulmonary embolism (PE), you will be given either unfractionated
heparin or low-molecular weight heparin together with warfarin for
the first few days (up to 1 week) until your blood test shows that
the warfarin dosage is effective.
|
|
Side effects
|
| |
warfarin is associated with a risk of
bleeding complications. It may also cause rash, nausea and
diarrhea. If you experience any side effects, you must consult
your physician. Warfarin should be avoided during pregnancy.
|
|
|
Potential drug interactions
|
|
|
Drug interactions with
warfarin can increase the anticogaulant effect which can
result in bleeding, or decrease the anticoagulant effect
which can lead to an increased risk of DVT. The following
are some of the most important drugs with which warfarin
interacts:
|
|
nonsteroidal anti-inflammatory
drugs
|
|
|
oral hypoglycemics (diabetes
drugs)
|
|
|
sulfonamides
|
|
|
antibiotics
|
|
|
drugs affecting liver enzymes
(e.g. some cholesterol-lowering drugs, such as carbamazepine)
|
|
|
corticosteroids
|
|
|
imidazole antifungals (e.g. Amfotericin
B, Fluconazole)
|
|
|
vitamin K in food (foods that
contain high levels of vitamin K include spinach,
avocado and cabbage), and dietary supplements (vitamin
K helps produce some important blood-clotting factors
and decreases the effects of warfarin).
|
|
|
Hormonal
contraceptives in general |
You should inform your physician
if you are taking any of these drugs or dietary supplements
and you are prescribed warfarin. You should also consult
your physician for more complete advice on the drugs likely
to interact with warfarin, and whether it is necessary to
adjust your diet in order to avoid foods high in vitamin
K.
|
|
|
Monitoring of therapy |
| |
If you are prescribed warfarin, you will
usually be monitored frequently and closely to minimize
the risk of serious bleeding complications. Your physician
may also periodically conduct a blood test (PT/INR) to ensure
that you are receiving the correct dose of warfarin. The
standardized method for reporting the results of this test
is called the international normalized ratio (INR). The
aim of your treatment will be to keep your INR within a
certain range.
|
Other treatment options
Other treatment options for deep-vein
thrombosis or pulmonary embolism (PE)
include thrombolytic therapy, thrombectomy and inferior vena cava
interruption.
Thrombolytic medications
Thrombolytic medications break down the blood
clot, i.e. they cause the clot to disintegrate. They are usually
used in combination with anticoagulant. These agents are very expensive
and are associated with a high incidence of bleeding. They are not
necessary for most patients with pulmonary embolism, but can be
life-saving in patients with a very large pulmonary embolism that
obstructs the flow of blood to the lungs.
Thrombectomy
Thrombectomy is the surgical removal of a thrombosis.
This technique is of limited use for blood clots in veins and is
50% successful in preventing a further thrombosis.
Inferior vena cava interruption
Partial interruption of the inferior vena cava
(the vein that carries blood from the lower body to the right side
of the heart) using clips, sutures (stitches) or filters prevents
the blood clot from reaching the lung. This technique is usually
considered in situations where anticoagulant medication cannot be
used because of bleeding, or in situations of repeated thrombosis
despite the use of antithrombotic medication.
|